
Prior authorization (PA) has long been a sticking point in healthcare: a process meant to ensure appropriate care often turns into a source of frustration for clinicians, patients, and payers alike. With mounting regulatory demands from CMS and state agencies, the need for modernization has never been more urgent.
In a recent joint webinar, UiPath and Genzeon explored how intelligent automation and agentic AI can revolutionize prior authorization, not only helping payers meet compliance deadlines but also transforming clinical operations for the long term.
Compliance or Transformation? The Industry’s Fork in the Road
 Vinit Singhal, who leads payer initiatives at Genzeon, set the stage:
Vinit Singhal, who leads payer initiatives at Genzeon, set the stage:
“We see payers in two camps—those treating PA as a compliance checkbox, and those who view it as a transformational opportunity for clinical operations. The latter are investing strategically, and they’re already reaping the benefits.”
The CMS Final Rule 0057 has created urgency by requiring prior authorization APIs by January 2027. Yet, as UiPath’s panelists noted, the challenge is not just about technology—it’s about redesigning workflows to ease the administrative burden on clinicians while meeting transparency and turnaround-time requirements.
The Clinician Perspective
One recurring theme was clinician burnout. As Sophia Pruitt, Senior Solutions Engineer from UiPath, noted:
“We hear the same challenges over and over: clinicians are burned out, turnaround times are too long, and processes are fragmented across multiple portals and faxes. Automation done right addresses these challenges directly.”
Instead of scrolling through hundreds of pages of medical records, clinicians can now receive AI-powered summaries that highlight exactly where medical necessity criteria are met. This saves hours of manual review while improving accuracy and patient care.
Quick Wins That Build Momentum
The speakers outlined several areas where payers can see immediate results:
- Intake Automation: Digitizing faxes and other submissions, classifying requests, and extracting key details.
- Case Building: Automatically populating systems with complete request information.
- Communication Generation: Using AI to draft patient- and provider-facing correspondence in plain language.
Sophia emphasized:
“Quick wins are important—but they must fit within a platform strategy. Otherwise, you risk point solutions that don’t scale.”
A Platform Approach, Not Point Solutions
Harsh Singh from Genzeon added a note of caution:
 “Some organizations pursue quick wins in isolation, but without a platform approach, those investments can backfire. You need a foundation where automation, agentic AI, and human review build on each other.”
“Some organizations pursue quick wins in isolation, but without a platform approach, those investments can backfire. You need a foundation where automation, agentic AI, and human review build on each other.”
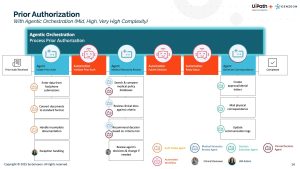
This layered model includes:
- RPA bots for deterministic, rules-based tasks like intake and system updates.
- Agentic AI for decision support—summarizing clinical records, comparing against guidelines, and triaging complexity.
- Human-in-the-loop oversight to ensure accuracy, avoid inappropriate denials, and maintain compliance.
Demonstrating the Art of the Possible
The webinar featured live demos showing how automation and AI work together:
- Faxed PA requests were digitized, classified, and automatically populated into payer systems.
- Medical necessity review agents surfaced clinical guidelines alongside highlighted evidence in patient records.
- Decision submission agents generated compliant correspondence and updated systems automatically.
Clinicians in the demos could see side-by-side records and AI-suggested criteria matches—a feature that panelists noted “clinicians actually get excited about.”
Guardrails and Governance Matter
The conversation also addressed a hot industry concern: AI-driven denials. Hersh stressed the importance of governance:
“We’ve seen negative press about AI increasing denial rates. That happens when there aren’t guardrails in place. Our approach emphasizes augmentation, transparency, and compliance—not replacement of clinical judgment.”
Real-World ROI
For payers questioning whether these solutions deliver value, the panelists were clear:
“Today we’re delivering engagements where ROI is not just theoretical—it’s guaranteed in outcome-based models. The automation pays for itself, and more.”
Building Toward the Future
With over 20 prebuilt clinical agents in development—from DME to oncology—Genzeon and UiPath stressed that these solutions aren’t hypothetical. They are live, in production, delivering measurable results today.
Bottom line: Prior authorization reform is inevitable. Whether payers approach it as a compliance exercise or a transformational opportunity will define their competitiveness and their clinician and member experience. With UiPath and Genzeon, the tools to make that transformation real are already here.
Frequently Asked Questions
CMS has finalized rules (e.g., CMS-0057-F) requiring payers to streamline prior authorization processes. Key changes include tighter response times, transparency requirements, and mandated adoption of standardized APIs for electronic submission and status tracking.
The major deadlines start in January 2026–2027, with different dates for implementing APIs, interoperability standards, and turnaround time expectations. Payers should be actively preparing now to meet compliance.
Medicare Advantage organizations, Medicaid and CHIP managed care plans, state Medicaid agencies, and Qualified Health Plan issuers on the federally facilitated exchanges. Many commercial plans have voluntarily agreed to meet the same deadlines, but are not covered by the CMS rules.
Payers must provide clear, specific denial reasons, publish metrics (such as approval/denial rates and turnaround times), and make prior authorization information publicly accessible.


