WISeR is built to make reviews more predictable and less burdensome, while aligning with existing Medicare rules.
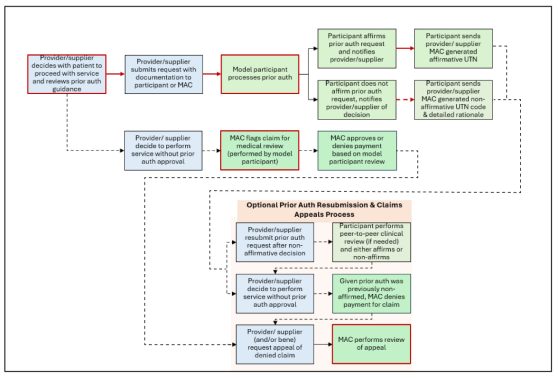
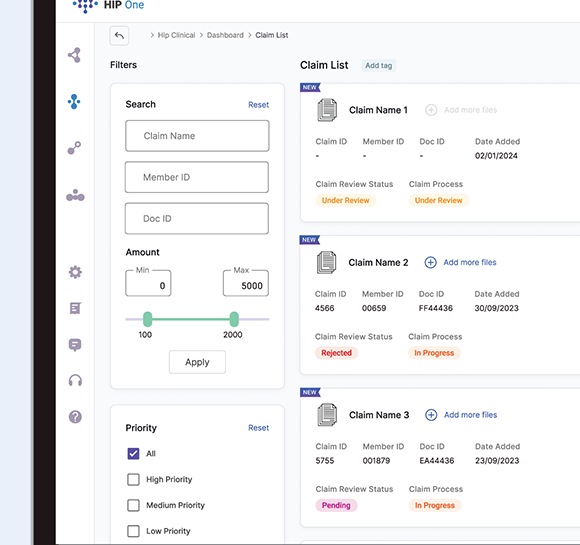
WISeR Request Process:
- Provider submits a prior authorization (PA) request for a WISeR-included service rendered in New Jersey.
- Technology-enhanced review flags completeness.
- Review checks documentation against current Medicare coverage criteria.
- Human clinical validation occurs when needed to confirm medical necessity.
- Determination returned within CMS-defined timeframes.
If a claim is submitted without required PA, it may enter pre-payment medical review.