Who We Help
Turning Challenges into Wins: How We Deliver Measurable Impact
The healthcare payer landscape is evolving rapidly—with AI breakthroughs, mega-mergers, and stringent regulations reshaping the industry. At Genzeon, we help payers stay ahead by reducing administrative burdens, improving member experiences, and driving cost efficiency through AI-powered automation and data intelligence.
![]() Source: PwC
Source: PwC
8% Healthcare Cost Surge Annually for Group Markets.
With AI and automation, we optimize operations to cut inefficiencies and deliver measurable savings.
![]() Source: Deloitte
Source: Deloitte
63% of Compliance Focus is Prioritized Under Health Plans
Our CompliancePro Solution simplifies adherence to evolving regulations, easing administrative burdens.
![]() Source: AMA
Source: AMA
85% Authorization Delays and Inefficiencies
Our HIP One platform automates workflows, speeding up approvals and reducing denials.
Our Platform
Our Healthcare Intelligence Platform
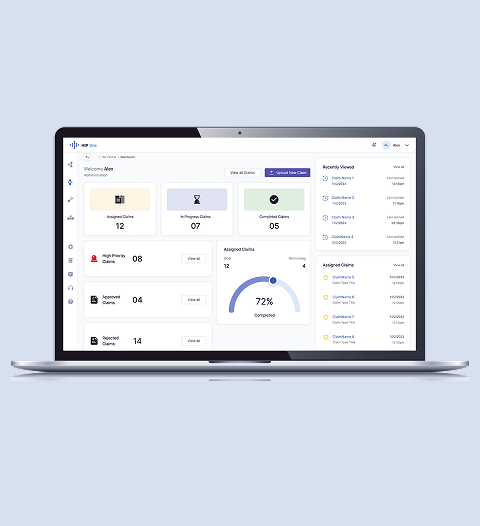
HIP One
The all-in-one platform that transforms healthcare operations with AI-powered automation, boosting efficiency and security.
- 42% Increased Productivity
- Secure clinical decision support
- Streamlined healthcare workflows
- AI-driven document handling
- Privacy-first construction
Case Studies
Stories That Inspire
What Sets Us Apart
Testimonial
What Our Clients Say
Frequently Asked Questions
Genzeon helps payer organizations reduce administrative workload, manage rising costs, and improve member experience. Through automation, data solutions, and compliance support, payers can streamline operations, strengthen governance, and achieve measurable results.
The Payers page highlights several use cases: Utilization Management and Prior Authorization, Provider Referral Management, Medicare Star Rating and HEDIS Measures, Complex Claim and Medical Review, and Patient Engagement and RCM. Each solution targets efficiency and accuracy in core payer functions.
HIP One is an all-in-one platform built to enhance healthcare operations with automation, secure document handling, and analytics. It enables faster approvals, higher productivity, and improved compliance while maintaining a privacy-first design.
Genzeon combines healthcare-exclusive expertise with technology-driven results. The company focuses on member-first solutions, operational excellence, and proven value—delivering lower costs, higher ROI, and measurable impact for payer organizations.
Upcoming Events